Hyperthermia, Seizures, and SCN1A Mutation Combined May Cause Sudden Death in Dravet Patients, Case Report Suggests
A combination of high body temperature, seizures, and SCN1A mutations can cause the rapid accumulation of fluid in the brain and cardiac arrest, potentially leading to sudden death in Dravet syndrome patients, according to a case report.
The study, “Can the combination of hyperthermia, seizures and ion channel dysfunction cause fatal post-ictal cerebral edema in patients with SCN1A mutations?” was published in the journal Epilepsy & Behaviour Case Reports.
The report describes the case of a 21-year old Dravet patient who died after experiencing a generalized convulsive seizure that resulted in fatal brain edema — abnormal accumulation of fluid in the brain.
The patient carried an SCN1A mutation, the most common gene mutation linked to Dravet, and had been diagnosed with this syndrome in childhood.
Cases of fatal cerebral edema in patients with SCN1A mutations, after a fever and repeated seizures without recovery between attacks, have recently been reported, raising the question of whether dysfunction in the sodium channel — for which the SCN1A gene provides instruction — may contribute to this condition and lead to an increased risk of premature death in Dravet patients.
The individual had been seizure-free for seven years, and was being treated with a combination of topiramate (sold under the brand names of Qudexy, Topamax, and Trokendi) and potassium bromide.
On the day he was admitted to the hospital, he had been running when a convulsive seizure started. Although he was immediately treated with oral midazolam (brand name Versed) and the seizure stopped, he went into cardiac arrest. After several cardiopulmonary resuscitation attempts, the patient did not survive.
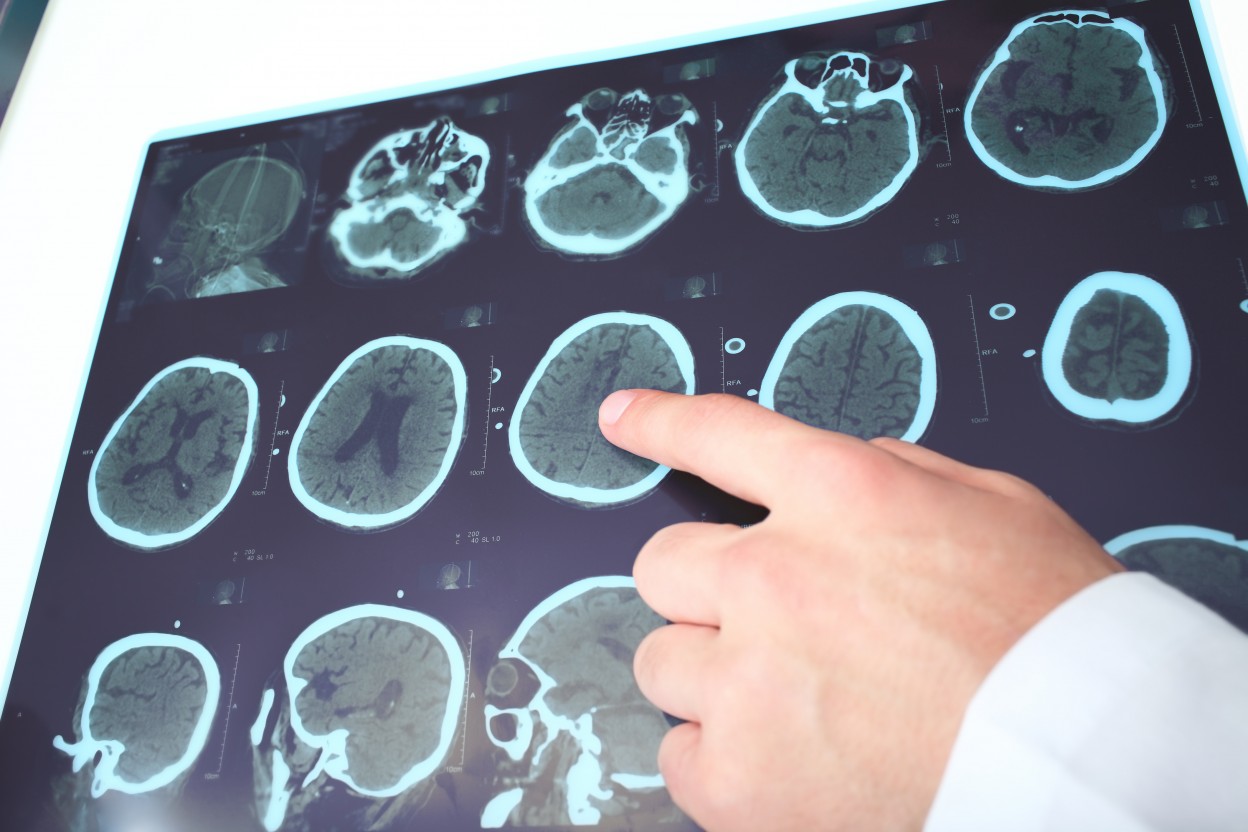
Computed tomography (CT) scans revealed that fluid had rapidly accumulated in the patient’s brain, leading to compression of his brain temporal lobe. This process happened within three hours after the seizure occurred. However, no brain injury or lesions were detected.
Researchers believe that this might have been a case of sudden unexpected death in epilepsy (SUDEP) due to fatal brain edema.
SUDEP is the leading cause of death related to epilepsy, and Dravet patients are at a particularly high risk. However, due to its abrupt and unexpected nature, it is difficult for clinicians and researchers to determine its cause.
Brain edema had previously not been considered to be a cause of SUDEP, but this report suggests that it actually might be involved in certain situations.
“We […] find it relevant to report on this case and bring to attention that there may be circumstances under which fatal cerebral edema develops rapidly in patients with DS [Dravet dyndrome],” the researchers wrote.
Researchers believe that brain edema occurred due to a combination of hyperthermia — high body temperature — and sodium channel dysfunction.
It is known that high body temperature, sodium channel dysfunction, and emotional stress may trigger seizures in Dravet patients. According to researchers, in this particular case, it is likely that the seizure was triggered by a prolonged state of high body temperature caused by intense physical activity on a warm day.
The fact that the patient was taking topiramate, which can reduce sweating and raise body temperature, might have contributed as well.
Importantly, hyperthermia might also have induced the fatal accumulation of fluid in the brain that followed the seizure. There are reports of an association between fever-related seizures and fatal brain edema in children with Dravet syndrome. However, the mechanisms connecting both occurrences are unknown.
During a seizure, there is excessive entry of sodium and calcium inside nerve cells. This process can lead to fluid accumulation in the brain and neuronal death. In Dravet patients who have defects in the SCN1A sodium channel, this process might be aggravated.
Therefore, under some circumstances, SCN1A mutations can contribute to fatal edema during the recovery period after a seizure.
“The combination of hyperthermia, ion channel dysfunction and possibly emotional stress may therefore not only trigger seizures but also facilitate a fatal pathophysiological cascade of cerebral edema leading to cerebral herniation causing cardiorespiratory collapse,” the researchers concluded.