Respiratory Impairments Common, May Increase Risk of Sudden Death in Dravet Syndrome, Study Finds
Severe respiratory abnormalities induced by seizures are common in patients with Dravet syndrome, and may increase patients’ risk of sudden unexplained death in epilepsy (SUDEP), according to a recent study.
The report, “Severe Peri-Ictal Respiratory Dysfunction is Common in Dravet Syndrome,” was published in The Journal of Clinical Investigation.
Dravet syndrome patients have a high risk of SUDEP. Several reasons have been proposed as the cause of SUDEP in these patients, mostly pointing to cardiac causes.
However, “measurements of breathing have not been made during spontaneous or heat-induced seizures” in mouse models of Dravet syndrome, so it remained unknown whether abnormal breathing contributes to SUDEP.
Researchers evaluated the potential contribution of breathing dysfunction after a seizure (called postictal) to SUDEP by analyzing patients and a mouse model of Dravet syndrome.
They reviewed video recordings of seven patients with Dravet syndrome and seven patients with localization-related epilepsy and saw that Dravet patients were more prone to have seizure-related abnormal breathing. These happened at the same time as disturbances in respiratory rhythm generation.
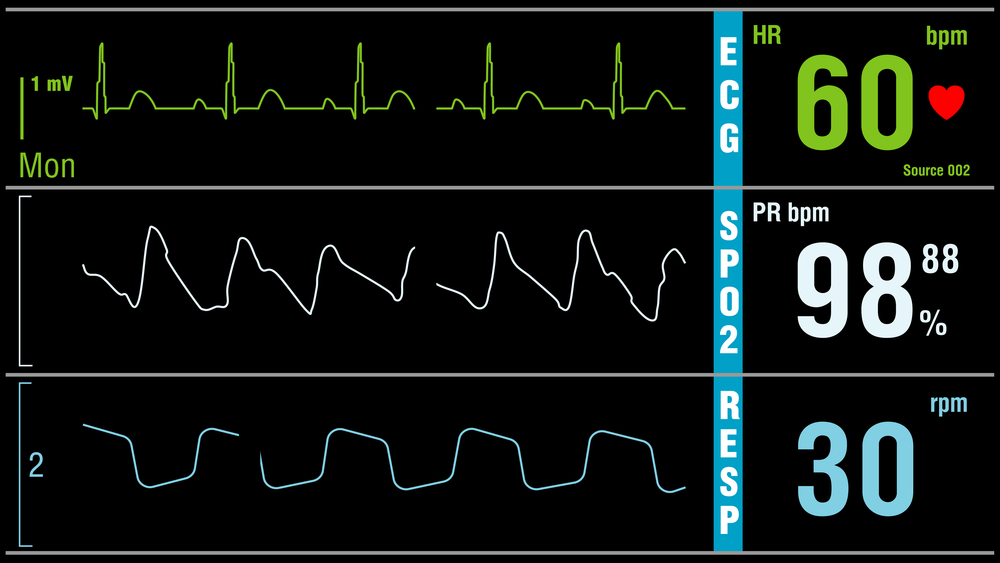
In one patient with Dravet syndrome, a 9-year old girl, researchers reviewed video-electroencephalography (EEG) monitoring and observed a severe and prolonged abnormal and poor respiratory activity (hypoventilation) following a seizure. The patient eventually died of SUDEP.
Researchers show that seizures in patients with Dravet syndrome induce breathing dysfunction – known as peri-ictal breathing dysfunction – lasting as long as four hours after the seizures end.
“In the non-fatal episodes documented here, these changes were transient, but the severe defects in breathing in the patient who later died of SUDEP suggest that respiratory changes may be biomarkers of patients at high risk,” they wrote.
They then used a mouse model of Dravet syndrome (in mice with a mutation described in three unrelated Dravet syndrome patients) to find the cause of death after the seizures.
The results showed that the mice “died after spontaneous and heat-induced seizures due to central apnea [their breathing stopped] followed by progressive bradycardia [a slow heart rate].”
Treatment with high doses of atropine, a muscarinic receptor antagonist, prevented death by blocking central apnea.
“These results indicate that atropine analogues have effects in the central nervous system that prevent seizure-induced apnea,” researchers wrote.
Overall, “cardiac abnormalities clearly play an important role in many cases of SUDEP, likely including some cases of [Dravet syndrome],” researchers explained.
But focusing only on cardiac changes is potentially misleading if not “evaluating breathing and blood gases, since changes in O2, CO2 and pH can induce a variety of cardiovascular abnormalities including bradycardia and tachyarrhythmias,” they added.
“This is of practical clinical importance, since a cardiac pacemaker would not be appropriate for preventing SUDEP in a patient with bradycardia secondary to central apnea. Instead, interventions that restore ventilation would be more logical for rescuing epilepsy patients who have peri-ictal respiratory arrest,” the study concluded.