Modulator of certain GABA-A receptors shows promise in model
KRM-II-81 being developed for future clinical trials for epilepsy, anxiety
A molecule designed to enhance activity at certain GABA-A receptor proteins in the brain protected against seizures and eased anxiety in a mouse model of Dravet syndrome, recent research showed.
At higher doses, the medication led to sedative side effects, which scientists believe can be avoided by making sure the right dose is established.
Called KRM-II-81, the molecule is now being further developed in preparation for future clinical trials in people with epilepsy and anxiety disorders, according to the authors.
“Our findings may lead to novel, pragmatic therapeutic strategies for DS [Dravet syndrome],” the researchers wrote. “For future clinical application, a pursuing for optimized dose should be important.”
The study, “Therapeutic effects of KRM-II-81, positive allosteric modulator for α2/3 subunit containing GABAA receptors, in a mouse model of Dravet syndrome,” was published in Frontiers in Pharmacology.
In Dravet syndrome, mutations in the SCN1A gene lead to a shift in the brain’s usual excitatory/inhibitory balance. Excitatory signals are ones that promote nerve cells’ electrical firing, whereas inhibitory signals reduce the odds of such firing.
An excess of excitatory signals and dysfunction of inhibitory networks that balance them leads to large number of nerve cells firing repeatedly and synchronously. Such an electrical pattern is consistent with seizures — the hallmark symptom of Dravet.
GABA is the main inhibitory signaling chemical, or neurotransmitter, in the brain. Treatment approaches to enhance GABA signaling are thus considered a promising way of controlling seizures for Dravet patients.
Indeed, some standard Dravet medications, such as Onfi (clobazam) and diazepam (e.g., Diastat), work to enhance GABA activity by binding to GABA-A receptor proteins, where the neurotransmitter normally exerts its effects, and boosting its activity. This is called a positive allosteric modulator, or PAM.
Such medications also can cause certain side effects, such as motor impairments or sedation that are related to increased inhibitory signaling.
GABA-A receptors can contain multiple types of subunits. It’s generally believed that the alpha-2/3 (a2/a3) subunits mediate anti-seizure effects, whereas the alpha-1 subunit could be involved in side effects.
Thus, a PAM specifically designed to only activate a2/a3-containing GABA-A receptors could offer a safe and effective strategy for treating Dravet. One such molecule, called KRM-II-81, has been found to have anti-epileptic effects in rodent models of epilepsy, with fewer sedative effects than diazepam.
Effects of KRM-II-81 in mouse model examined
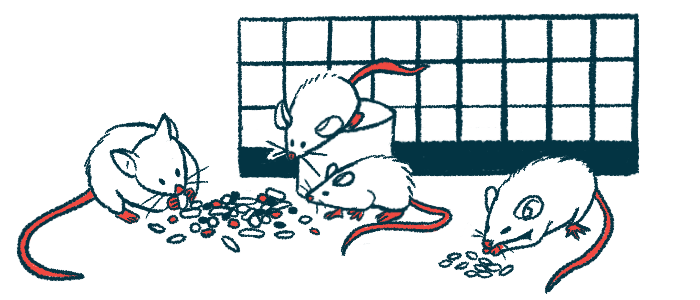
In the study, the researchers examined the effects of KRM-II-81 in a mouse model of Dravet syndrome, where mice are genetically engineered to house a known Dravet-causing mutation in the Scn1a gene.
Fever-induced seizures are a key symptom of Dravet. Consistently, the mouse model exhibits an increased susceptibility (reduced threshold) to temperature-induced seizures.
A single subcutaneous (under-the-skin) injection of KRM-II-81 led to significant and dose-dependent increases in seizure threshold for juvenile Dravet mice, meaning they were less likely to have seizures at temperatures where untreated mice would.
A low dose of the therapy also reduced anxiety-like behaviors in adult Dravet mice. However, a higher dose treatment caused the mutant mice, but not healthy mice, to have decreased overall locomotor activity and reduced paw grip strength, possibly indicating dose-dependent sedative side effects.
These differences between the Dravet and healthy mice suggested to the researchers that KRM-II-81 may have different effects on GABA-A receptors in the two types of mice.
In brain slices from the mice, the team indeed observed that KRM-II-81 more efficiently boosted spontaneous inhibitory signaling at nerve cell junctions in the Dravet mice compared to healthy ones, suggesting they may be more sensitive to the therapy.
“Selective activation for [a2/a3-containing GABA-A receptors] by KRM-II-81 could be potential therapeutic strategy for treating seizures and behavioral problems in [Dravet],” the researchers wrote.
Given the possible sensitivity to such medications, “slow titration … would be particularly important for planning its administration protocol,” the team added.
Future studies also will need to investigate whether chronic administration of the therapy affects this sensitivity.