Body Cooling May Shorten Refractory Seizures in Dravet and Other Epilepsies
Written by |
Used in addition to standard treatments, therapeutic hypothermia — based on lowering the body’s temperature — can shorten the duration of long-lasting seizures in drug-resistant forms of epilepsy, including Dravet syndrome, a study finds.
The study, “Therapeutic hypothermia for pediatric refractory status epilepticus May Ameliorate post-status epilepticus epilepsy,” was published in the Biomedical Journal.
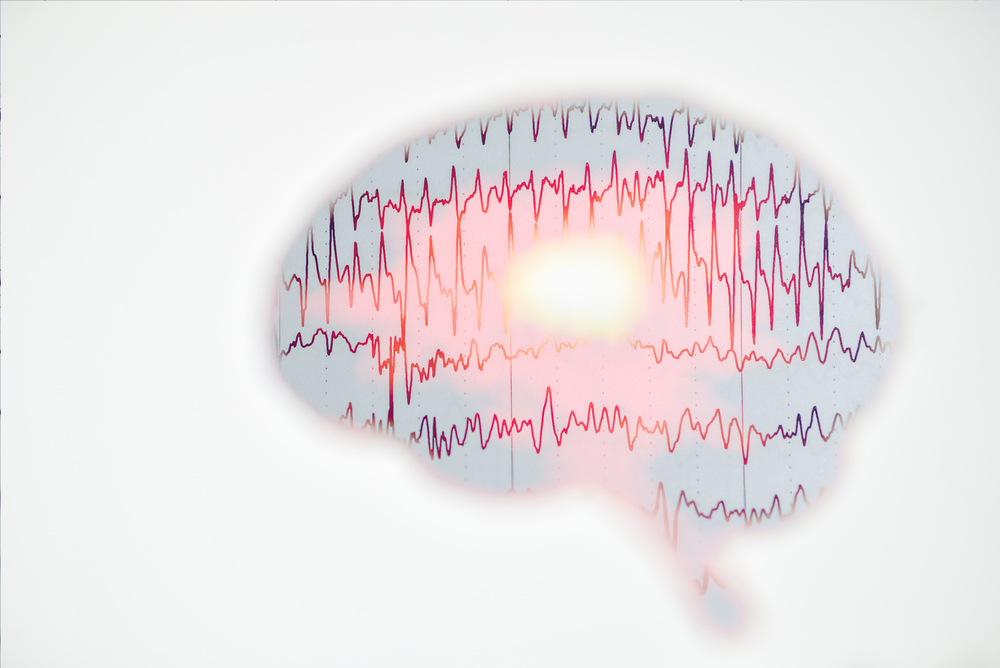
Dravet syndrome is a severe type of epilepsy that usually manifests early on in life. It is characterized by convulsive seizures that typically fail to respond to treatment with anti-epileptic drugs (AEDs).
Refractory status epilepticus (RSE) and super-refractory status epilepticus (SRSE) are two of the most severe types of drug-resistant convulsive seizures.
RSE seizures are those lasting more than one hour despite treatment with first- and second-line AEDs, while SRSE seizures last or return over a period of more than 24 hours after the patient is placed under general anesthesia.
Both RSE and SRSE seizures are normally managed with anesthetic agents like propofol, midazolam, barbiturate, or ketamine.
“Unfortunately, these medications only achieve [a therapeutic] effect in 64–78% of patients. Thus, alternative therapeutic approaches with better efficacies are needed for patients with RSE/SRSE,” the researchers wrote.
Therapeutic hypothermia (TH), a form of therapy used to prevent organ and neuronal damage, has previously been used as a complementary treatment for RSE seizures.
However, studies assessing TH’s effectiveness in controlling seizures have had variable results, particularly those concerning children.
A team of researchers in Taiwan carried out a retrospective study to compare clinical outcomes between a group of children experiencing RSE/SRSE seizures and given TH therapy with a group who were not.
They reviewed the medical records of 23 children with RSE/SRSE seizures who were admitted to the pediatric intensive care unit (PICU) of the Taoyuan Chang Gung Children’s hospital and Kaohsiung Chang Gung Memorial Hospital between January 2014 and December 2017.
Of the 23 children included in the study, 11 received TH in combination with anticonvulsants to control seizures, and 12 received anticonvulsants only (control group).
TH was applied using Medivance’s Artic Sun temperature management system with Artic Gel pads that were placed over the patients’ skin. Treatment was applied for 48 to 72 hours, until patients’ body temperature dropped to 34–35 C (93–95 F).
Investigators assessed and compared the duration of RSE/SRSE seizures, the time patients remained in the pediatric intensive care unit, and scores of the Glasgow Outcome Scale (GOS; a measure of neurological impairment) in both patient groups.
Of the 11 children who received TH in combination with anticonvulsants, seven had febrile infection-related epilepsy syndrome (FIRES), one had Dravet syndrome, and three a traumatic brain injury. More than half (58.13%) of the children in the control group had also been diagnosed with FIRES.
Children given therapeutic hypothermia as an add-on therapy had shorter seizures compared to those who only received anticonvulsants (a median of 24 hours vs. 96 hours).
Moreover, children in the TH group had higher GOS scores compared with those in the control group (a median of 4 vs. 3), indicative of milder neurological impairments and better long-term clinical outcomes.
Later chronic refractory epilepsy was reported in less than half (45%) of the TH group children, whereas all in the control group developed this form of epilepsy after one year of follow-up. Duration of stay in a pediatric intensive care unit was similar in both groups.
The child with Dravet, an 8-year-old boy, developed “refractory SE [status epilepticus] due to an influenza infection,” with poor response to AEDs because of a persistent high fever. “We applied TH along with continuous midazolam infusions. … The patient recovered well after rewarming, without cognition or motor function deteriorations,” the researchers wrote.
“Collectively, our findings support that TH effectively shortens the seizure duration in pediatric patients with RSE/SRSE,” they concluded.
Apart from electrolyte imbalances, which were manageable, therapeutic hypothermia was found to be “safe for use in pediatric patients with RSE/SRSE.” (Electrolytes are minerals in the blood and other body fluids, such as calcium, magnesium or phosphate, that carry an electric charge and are necessary for muscle function, blood acidity, and other key processes.)
“Our study provides evidence that shortened seizure durations in the acute symptomatic phase of SE can reduce the occurrence of post-status epilepticus epilepsy and improve patients’ long-term functional outcomes,” the researchers added.