Patient-derived ‘mini-brains’ may aid study of Dravet syndrome
Induced pluripotent stem cells were used to develop organoids of affected brain regions
Written by |
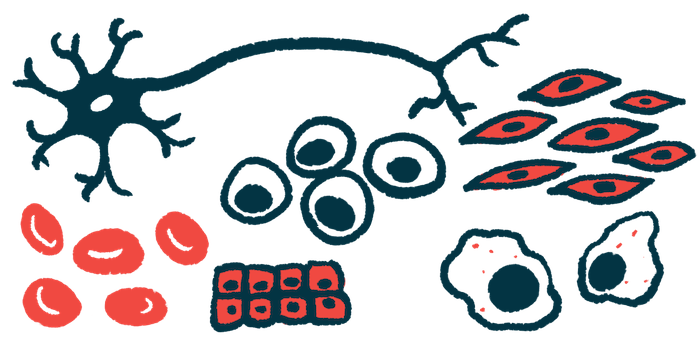
Brain-like organoids, or “mini-brains,” that are specific to affected brain regions and derived from patients could act as models for studying the underlying molecular mechanisms of Dravet syndrome, a study shows.
Researchers created patient-derived organoids of the forebrain, a region enriched with types of nerve cells called GABAergic neurons that are the most affected in Dravet.
They found changes in molecules involved in mitochondria (the cell’s powerhouses), supporting previous preclinical studies suggesting mitochondrial impairment contributes to Dravet.
“The [Dravet syndrome] organoid model will provide an additional resource for deciphering the [mechanisms] behind Nav1.1 [deficiency] and drug screening to remediate the functional deficits associated with the disease,” the researchers wrote in the study, “The Generation of Human iPSC Lines from Three Individuals with Dravet Syndrome and Characterization of Neural Differentiation Markers in iPSC-Derived Ventral Forebrain Organoid Model,” which was published in Cells.
Dravet syndrome is a rare type of epilepsy marked by prolonged seizures that start in early childhood and are difficult to control with anti-seizure medications. In 80-90% of cases, the disease is caused by mutations in the SCN1A gene, which encodes a subunit of a sodium channel called NaV1.1. This sodium channel is found on the surface of nerve cells and controls the entrance of sodium ions into them, which is required to activate them so they can communicate with other nerve cells.
This communication depends on a fine balance between excitatory and inhibitory signals. Excitatory signals from one nerve cell to the next make the latter more likely to fire an electrical signal, while inhibitory signals make it less likely to fire.
How SCN1 mutations result in seizures is not fully understood, but scientists believe the impaired function of inhibitory GABAergic neurons may be implicated.
“This would result in the overactivation of the nervous system, the transmission of signals uncontrollably, and the development of seizures,” the researchers wrote.
One of the major limitations in understanding the molecular mechanisms behind Dravet is the lack of a cellular model that fully replicates the disease’s complexity, however.
Induced pluripotent stem cells, or iPSCs, are increasingly used to study diseases. They’re produced by collecting mature cells, such as in the skin or blood, and reprogramming them back into a stem cell-like state, where they can mature into virtually any cell type. They can be derived directly from patients for use as cellular models that mimic a disease’s genetic and clinical diversity.
Generating ‘mini-brains’ from stem cells
Researchers in Poland generated “mini-brains” from iPSCs derived from people with Dravet and with Panayiotopoulos syndrome (PS), a milder form of genetic epilepsy that also appears in early childhood.
Human “mini-brains” are three-dimensional brain-like organoids that can more fully mimic the properties and cellular interactions of the human brain than animal models. When derived from people with neurologic conditions, they can be used to replicate disease processes and help predict a therapy’s clinical benefit.
The researchers first generated iPSCs from skin cells of two people with Dravet syndrome and one with PS, all carrying distinct mutations in the SCN1 gene. The presence of the patients’ original mutations was confirmed in their corresponding iPSCs.
They then used iPSCs from one Dravet patient and the PS patient to mature them into organoids of the ventral forebrain, a region rich in GABAergic neurons.
The patient-derived iPSCs “reflected the severity of the symptoms in the respective donors, from mild to more severe clinical picture,” the researchers wrote.
Differences between Dravet, healthy donors’ ‘mini-brains’
In the Dravet patient-derived “mini-brains,” the levels of GABAergic neuronal markers were elevated compared with organoids from the PS patients and a healthy donor. These differences failed to reach statistical significance, though.
Ventral forebrain markers were significantly increased in Dravet “mini-brains” relative to those from healthy donors, while no significant differences were seen between healthy organoids and those from the patient with the milder epilepsy.
The fact that the organoids already had matured GABAergic neurons makes it “plausible to speculate that SCN1A mutations affect the inhibitory neurons after cell maturation since the sodium channel Nav1.1 is involved in signal transmission,” the researchers wrote.
Since previous evidence suggested mitochondrial dysfunction is involved in Dravet, the researchers looked at potential changes in mitochondrial markers.
They found significantly reduced activity of the PPARGC1A gene, a main regulator of mitochondria growth and function, in organoids from both patients compared with those from a healthy donor.
The levels of other mitochondrial markers were significantly increased in the Dravet “mini-brains” relative to healthy organoids, but not in those from the PS patients, which could reflect disease severity.
“Establishing brain-region organoids from donors afflicted with [Dravet syndrome] allows for studying the effect of the disease in a more complex environment, which should display changes reflecting the degree of severity of the underlying [disease mechanisms],” the researchers wrote. “This organoid model can be used to determine the stage of neural development at which the SCN1A gene [is activated], which would give the opportunities for intervention.”