Protein That Suppresses Seizures in Mice May Benefit Epilepsy Patients in Future
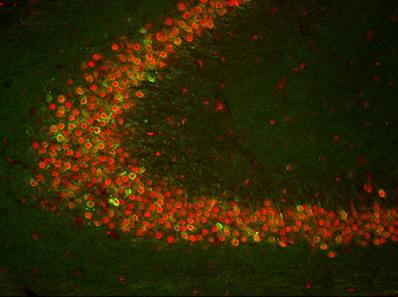
"TIA-1 is known for its ability to regulate gene expression during cellular stress,"James Hewett, associate professor of biology, said in a press release. "We suspected that TIA-1 was involved with seizure suppression, but our findings suggested something else." Credit: Courtesy of Elsevier
Increased brain levels of a protein involved in inflammation were found to suppress seizures in mice, a finding that may have potential for the treatment of types of epilepsy, including Dravet syndrome.
The study, “Maintenance of the Innate Seizure Threshold by Cyclooxygenase-2 is Not Influenced by the Translational Silencer, T-cell Intracellular Antigen-1,” appeared in the journal Neuroscience.
TIA-1 is a protein that acts in the cell nucleus to regulate gene expression during cellular stress. It is also involved in the control of cell death and division, as well as in mouse embryonic development.
Through its role on gene expression, TIA-1 participates in several processes related to disease, including antiviral, inflammatory, and immune responses.
Syracuse University researchers focused on brain TIA-1, whose function is not well understood. The scientists were also interested in the function of an enzyme called cyclooxygenase-2 (COX-2), which mediates the production of prostaglandins — inflammatory molecules involved in pain and fever.
To explore the role of TIA-1 and COX-2 in epilepsy and the extent to which TIA-1 regulates the levels of COX-2 in the brain, researchers used genetically modified mice with elevated levels of COX-2 in their nerve cells in an experimental model of convulsions.
“TIA-1 is known for its ability to regulate gene expression during cellular stress,” James Hewett, PhD, associate professor of biology and the study’s senior author, said in a Syracuse University news story written by Rob Enslin. “We suspected that TIA-1 was involved with seizure suppression, but our findings suggested something else.”
The data revealed that increased COX-2 levels in nerve cells suppressed seizures in mice.
“Our findings raise the possibility that the level of neuronal COX-2 expression in the brain may be a determinant of the seizure threshold,” Hewett said. The seizure threshold refers to a natural limit for electrical activity, above which seizures occur.
TIA-1 binds to COX-2 messenger RNA — a molecule generated from DNA in the first step of gene expression — and inhibits the production of the COX-2 protein in cells other than neurons.
This led scientists to hypothesize that complete elimination of TIA-1 would increase COX-2 production, which would increase resistance to acute seizures. However, results revealed that mice lacking TIA-1 had unchanged neuronal levels of COX-2 and also did not exhibit changes in their susceptibility to seizures.
“Cures and preventive measures remain elusive, and the incidence of resistance to antiepileptic drugs is a clinical limitation,” Hewett said.
A deeper understanding of the brain mechanisms associated with COX-2 “could identify approaches for the development of novel antiepileptic therapies that target enhancement of the level of COX-2 expression in neurons,” the researchers wrote.






